
A Quick Review of Antidepressant Induced Mania
Quick Literature Review
There are many case studies of SSRI induced mania, but minimal research on how to treat these patients (Joseph 2009). Moreover, the published chart reviews of AIM fail to present any compelling evidence of harm (Joseph 2009).
Among patients initially diagnosed with Major Depressive Disorder (MDD), those treated with antidepressants are more likely to experience mania or hypomania. In their 2009 meta-analysis of AIM, Tondo et al. found that of patients with MDD treated with antidepressants, 5.97% developed mania/hypomania. On the other hand, of the patients with MDD treated without antidepressants, only 1.24% developed mania/hypomania (Tondo 2009).
There are currently six research reviews published regarding AIM:
All of these studies encourage vigilant screening for risk factors in order to prevent new cases of AIM; however, in a risk verses benefit analysis, depression is worse than mania in terms of burden on the individual and risk of suicide (Joseph 2009). As a result, the current recommendation is to proceed with caution when prescribing antidepressants to those with the highest risk factors.
A Look at Risk Factors
- Previous antidepressant induced manias;
- Bipolar family history; and
- Past exposure to multiple antidepressant trials.
Furthermore, Akiskal et al. found that an elevated risk for AIM is also associated with
- A family history of suicide;
- A hyperthymic temperament;
- A greater chronicity of depression;
- More hospital admissions;
- More mood associated psychotic features; and
- History of ECT treatment.
Also, Altshuler et al. found that AIM was more common in:
- Female gender;
- Bipolar II subdiagnoses; and
- Patients with a history of alcohol abuse/dependence.
Finally, AIM is moderately associated with the serotonin-transport-linked promoter region polymorphism (Daray 2010).
Medication Selection
Children ages 10-14 are the most vulnerable to manic induction by any class of antidepressant (Lim 2005).
Simple Decision Algorithm
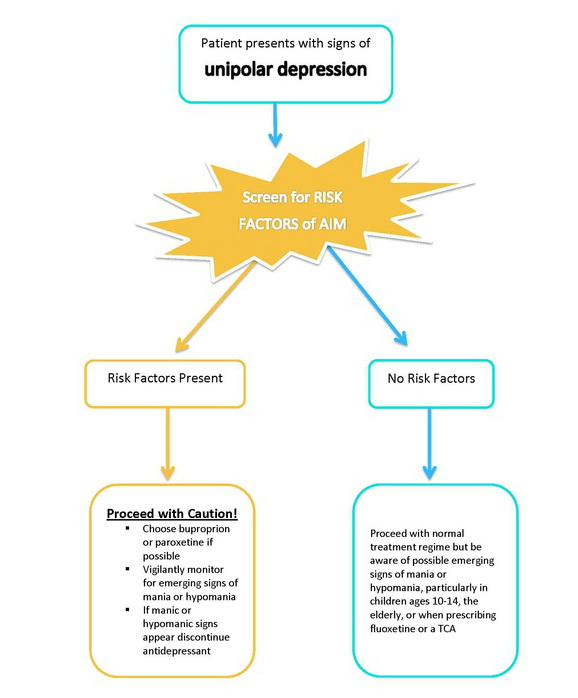
The best method for preventing new cases of AIM is to educate clinicians to recognize the patients with the highest risk factors. Once clinicians can accurately identify the at risk population, they can proceed with educated caution and be more vigilant to screen for emerging mania/hypomania.
Below is a simple algorithm used to manage AIM.
Martin A., Young C., Leckman J.F., et al. Age effects on antidepressant-induced manic conversion.Archives of Pediatric and Adolescent Medicine 2004; 158: 773-780.
0 Comments on "A Quick Review of Antidepressant Induced Mania"